Transarterial Chemoembolization (TACE)
Transarterial Chemoembolization (TACE): An Advanced Frontier in Cancer Care
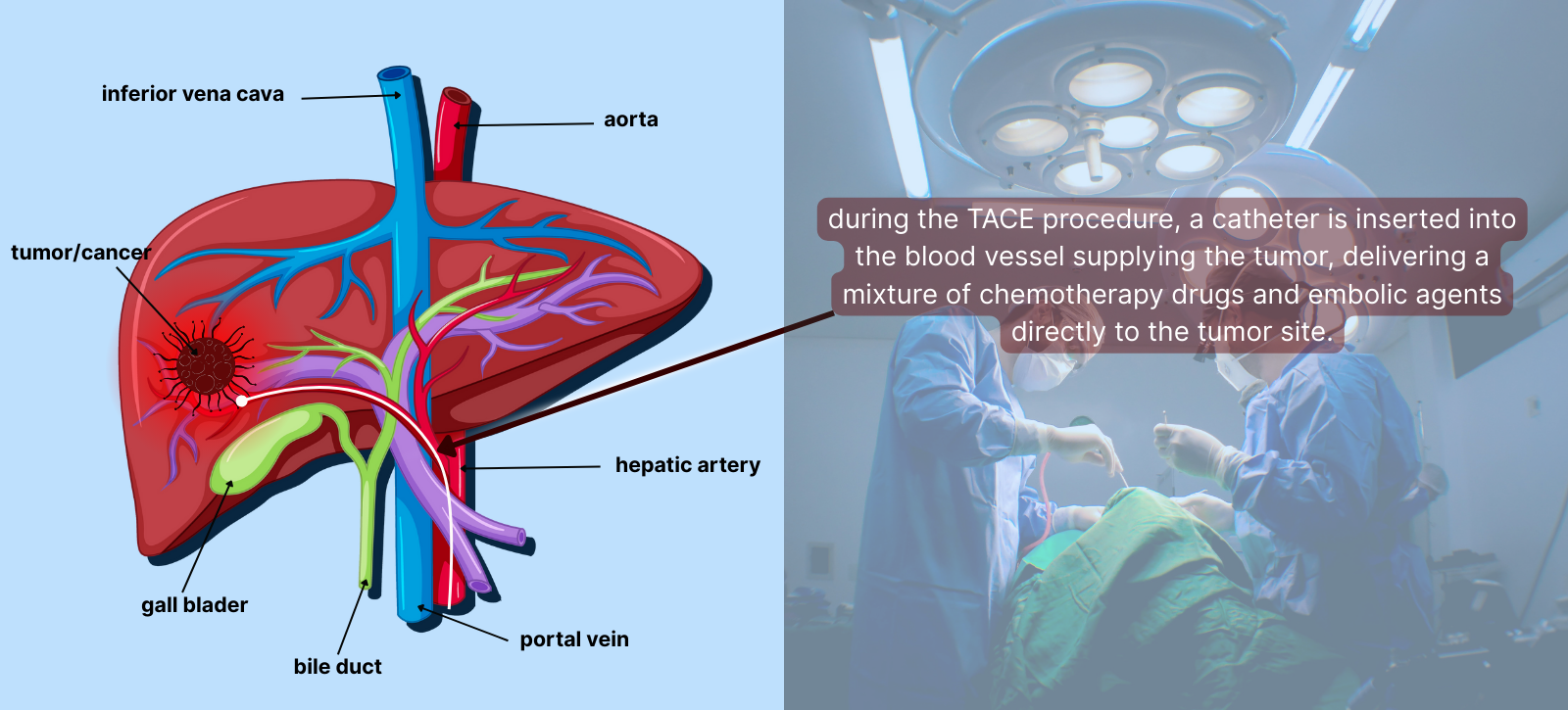
Transarterial Chemoembolization, commonly abbreviated as TACE, is a highly specialized, minimally invasive procedure that has transformed the therapeutic landscape for liver cancers, particularly hepatocellular carcinoma (HCC). Designed to selectively target tumors while sparing healthy tissues, TACE exemplifies the marriage of interventional radiology and oncology.
What is TACE?
TACE is a dual-action treatment that combines:
- Localized Chemotherapy:
- A potent chemotherapeutic agent (e.g., doxorubicin, cisplatin) is administered directly into the artery that feeds the tumor.
- This achieves drug concentrations at the tumor site that are many times higher than what could be safely achieved through systemic chemotherapy.
- Arterial Embolization:
- Tiny embolic particles (e.g., gelatin sponge particles, polyvinyl alcohol, or drug-eluting beads) are introduced to block the blood vessels supplying the tumor.
- By obstructing these arteries, the tumor’s oxygen and nutrient supply is severed, leading to ischemic necrosis (cell death).
This dual-action approach ensures that a high concentration of chemotherapy attacks the cancer cells locally, while the embolization starves the tumor of oxygen and nutrients, causing it to shrink or die.
Key Concept:
Liver tumors receive most of their blood supply from the hepatic artery, while normal liver tissue is mainly fed by the portal vein. TACE exploits this anatomical distinction, maximizing tumor targeting while minimizing damage to healthy liver tissues.
Why is TACE Globally Adopted?
TACE has become a gold standard in the treatment of intermediate-stage HCC and is also applied to other cancers (e.g., neuroendocrine tumors, colorectal cancer metastases) involving the liver. Its global adoption stems from:
- Enhanced Survival Rates: Studies have shown that TACE extends overall survival in patients with unresectable HCC compared to best supportive care.
- Palliative Benefits: TACE helps in reducing tumor size, alleviating symptoms like pain, bleeding, and portal vein compression.
- Adaptability: Suitable for a broad range of patients, including those awaiting liver transplantation (bridging therapy).
- Low Systemic Toxicity: Because the chemotherapy is confined to the tumor's vicinity, patients experience fewer systemic side effects.
Cutting-Edge Advances in TACE
- Drug-Eluting Bead TACE (DEB-TACE):
- Uses specially designed beads that absorb and slowly release chemotherapy.
- Provides a sustained drug release over days to weeks.
- Reduces systemic leakage of the drug, further limiting side effects.
- Balloon-Occluded TACE (B-TACE):
- Employs a microballoon catheter to temporarily occlude the artery during chemotherapy infusion.
- Increases local drug concentration and enhances embolization efficiency.
- Image-Guided Enhancements:
- Cone-Beam CT (CBCT): Real-time 3D imaging during the procedure ensures precise catheter navigation and monitoring of embolization.
- Fusion Imaging: Combines ultrasound and CT/MRI data for superior tumor targeting.
- Perfusion Imaging: Allows visualization of blood flow dynamics, guiding the intervention.
- Biodegradable Embolic Agents:
- Being developed to naturally dissolve after occluding the tumor vessels, reducing long-term risks like liver infarction.
Challenges and Future Directions
Ongoing clinical trials and technological innovations continue to expand the horizons of TACE. The integration of TACE with systemic immunotherapies and molecular-targeted agents holds promise for synergistic effects, potentially revolutionizing cancer care. Additionally, the refinement of biodegradable embolic materials and real-time monitoring of therapeutic responses are paving the way for safer, more effective treatments.
- Response Assessment: Tools like the modified Response Evaluation Criteria in Solid Tumors (mRECIST) are refining how we evaluate treatment success.
- Combination Therapies: Trials are exploring TACE with systemic therapies, such as immune checkpoint inhibitors (e.g., nivolumab) and tyrosine kinase inhibitors (e.g., sorafenib), to amplify therapeutic outcomes.
- Precision Medicine: Advances in genomics and biomarker profiling may soon allow personalized TACE protocols based on tumor-specific characteristics.
Transarterial Chemoembolization (TACE) stands as a cornerstone of interventional oncology, offering targeted, effective, and repeatable therapy for liver malignancies. As technology and medical research advance, TACE is poised to become even more precise and powerful, bringing renewed hope to patients with liver cancer worldwide.
